Back to Colorectal Cancer Brochures
Introduction
What is Hereditary Nonpolyposis Colorectal Cancer (HNPCC)?
What are Polyps?
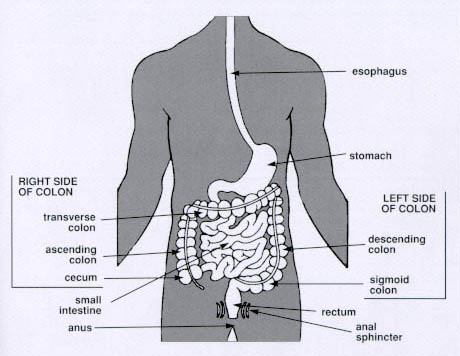
What is the Gastrointestinal Tract?
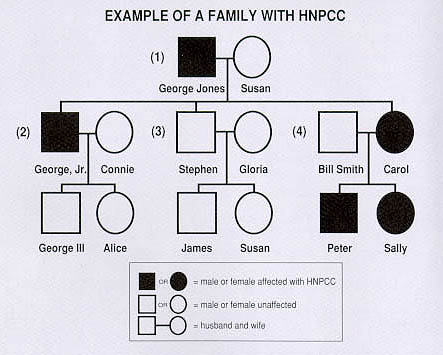
How is HNPCC Inherited?
DNA/Gene test for HNPCC
Why is Early Diagnosis Important?
Exam Guidelines for People at Risk
Exam Guidelines for People Who Have Had HNPCC Gene Testing
What are the Symptoms of HNPCC?
How is HNPCC Diagnosed?
What is the Treatment?
Sexual Function and Childbirth After Surgery
Follow-up Care After Surgery
Exam Guidelines for People With HNPCC Who Have Had Surgery
Support Groups for Individuals and Families
Resources
Publications
Glossary
Appendix: Guidelines for Early Detection of Cancer in People Not at Risk for HNPCC