| This booklet was prepared
by the following members of The Johns Hopkins Polyposis Clinic and Registry
in 1988, revised 1994: Susan Viles Booker, BA., Paul Celano, M.D., Donna
Cox, M.Ed., Susan Cross-Skinner, RN., M.S.N., Francis M. Giardiello, M.D.,
Pearl Campbell, B.S., Stanley R. Hamilton, M.D., Anne J. Krush, MS., L.
Stefan Levin, D.D.S., M.S.D., Gloria M. Petersen, Ph.D., Kathy Potter,
RN., Elias I. Traboulsi, M.D., and John Yardley, M.D.
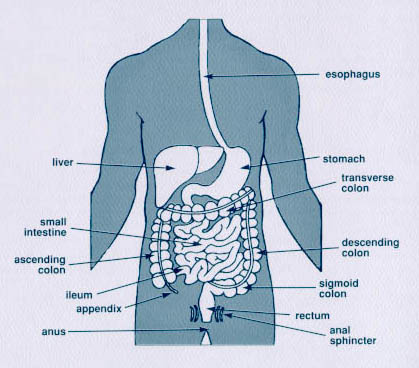
The gastrointestinal tract
illustration on page 3 was reprinted with permission of Bonnie Sue Rolstad,
R.N.,B.A.,E.T., from the booklet "Ileoanal Reservoir: A Patient Resource."
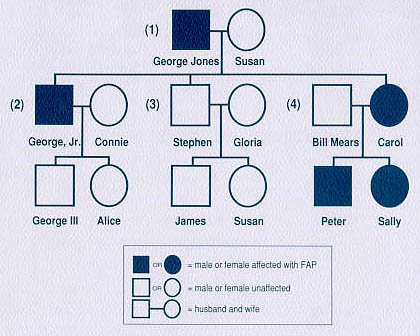
We would like to thank Linda
M. Welch for secretarial assistance, Theresa Berk, MS., for assistance
in compiling the glossary, and Joanna Strayer Amberger, BA. for technical
assistance on the pedigree illustration, page 5.
We would also like to thank
the Clayton Fund, The Johns Hopkins Oncology Centers Community Programs
and the Cancer Research Foundation of America for their support in the
development of this booklet.
Supported by Roche Biomedical
Laboratories, Inc.
To order copies of this
booklet, please contact the Coordinator, The Johns Hopkins Polyposis Registry,
Blalock 1008, The Johns Hopkins Hospital, 600 North Wolfe Street, Baltimore,
MD 21287-4922, phone (410) 955-3875.
© 1994 The
Johns Hopkins University
|